How to Get Pregnant with PCOS and High Testosterone: Understanding the Challenges
Polycystic ovary syndrome (PCOS) is a hormonal disorder that affects women of reproductive age. It is characterized by irregular periods, high levels of testosterone, and difficulty getting pregnant. High testosterone levels can interfere with ovulation, making it difficult for women with PCOS to conceive. However, there are several treatments available to help women with PCOS get pregnant.
This article will discuss the challenges of getting pregnant with PCOS and high testosterone, as well as the various treatment options available. We will also provide tips for managing PCOS and improving your chances of conceiving.
How to Get Pregnant with PCOS and High Testosterone
For women with PCOS and high testosterone, getting pregnant can be a challenge. However, there are a number of key aspects to consider that can improve your chances of conceiving.
- Hormonal balance
- Ovulation induction
- Weight management
- Insulin resistance
- Lifestyle changes
- Medications
- Surgery
- Assisted reproductive technologies
- Emotional support
By understanding these key aspects and working with your doctor, you can develop a treatment plan that is right for you and improve your chances of getting pregnant.
Hormonal balance
Hormonal balance is crucial for women with PCOS who are trying to get pregnant. When hormones are out of balance, it can interfere with ovulation and make it difficult to conceive. There are a number of different hormones that play a role in fertility, including estrogen, progesterone, and testosterone.
- Estrogen is a hormone that is produced by the ovaries. It is responsible for regulating the menstrual cycle and preparing the uterus for pregnancy.
- Progesterone is a hormone that is produced by the corpus luteum after ovulation. It helps to maintain the pregnancy by thickening the uterine lining and preventing the uterus from contracting.
- Testosterone is a hormone that is produced by the ovaries and adrenal glands. In women, testosterone levels are typically lower than in men. However, women with PCOS often have higher levels of testosterone, which can interfere with ovulation.
Hormonal balance is essential for fertility. By understanding the role of different hormones in the menstrual cycle and pregnancy, women with PCOS can take steps to improve their chances of getting pregnant.
Ovulation induction
For women with PCOS who are not ovulating on their own, ovulation induction may be a necessary step to get pregnant. Ovulation induction is a process of using medication to stimulate the ovaries to produce and release eggs.
- Clomid
Clomid is a medication that is commonly used to induce ovulation in women with PCOS. It works by blocking the estrogen receptors in the brain, which causes the pituitary gland to produce more FSH. FSH is a hormone that stimulates the ovaries to produce eggs.
- Letrozole
Letrozole is another medication that can be used to induce ovulation in women with PCOS. It works by inhibiting the production of estrogen, which allows the pituitary gland to produce more FSH.
- Gonadotropins
Gonadotropins are hormones that are produced by the pituitary gland. They are responsible for stimulating the ovaries to produce eggs. Gonadotropins can be used to induce ovulation in women with PCOS who have not responded to other medications.
- Surgery
In some cases, surgery may be necessary to induce ovulation in women with PCOS. Surgery can be used to remove the cysts that are blocking the ovaries from releasing eggs.
Ovulation induction can be a successful treatment for women with PCOS who are trying to get pregnant. However, it is important to note that ovulation induction can have side effects, such as multiple pregnancies, ovarian hyperstimulation syndrome, and birth defects. It is important to talk to your doctor about the risks and benefits of ovulation induction before starting treatment.
Weight management
Weight management is an important aspect of getting pregnant with PCOS and high testosterone. Maintaining a healthy weight can help to improve ovulation and fertility.
- Diet
Eating a healthy diet is essential for weight management. A healthy diet should include plenty of fruits, vegetables, and whole grains. It should also be low in saturated fat, cholesterol, and sodium.
- Exercise
Exercise is another important part of weight management. Exercise can help to burn calories and build muscle. It can also help to improve insulin sensitivity and reduce stress.
- Behavior modification
Behavior modification techniques can help you to change your eating and exercise habits. These techniques can help you to lose weight and maintain a healthy weight.
- Medication
In some cases, medication may be necessary to help you lose weight. Medication can help to reduce appetite or increase metabolism.
Weight management can be a challenge, but it is important for women with PCOS who are trying to get pregnant. By making healthy lifestyle changes, you can improve your chances of conceiving.
Insulin resistance
Insulin resistance is a condition in which the body does not respond properly to insulin. Insulin is a hormone that helps the body to use glucose for energy. When the body is insulin resistant, glucose builds up in the blood and can lead to a number of health problems, including weight gain, diabetes, and heart disease.
Insulin resistance is a common problem for women with PCOS. In fact, up to 70% of women with PCOS are insulin resistant. Insulin resistance can make it difficult to get pregnant because it can interfere with ovulation. Ovulation is the process by which an egg is released from the ovary. Insulin resistance can cause the ovaries to produce too much testosterone, which can block ovulation.
There are a number of things that women with PCOS can do to improve their insulin resistance. These include:
- Losing weight
- Eating a healthy diet
- Exercising regularly
- Taking medication
Improving insulin resistance can help to improve fertility in women with PCOS. By making healthy lifestyle changes and taking medication when necessary, women with PCOS can increase their chances of getting pregnant.
Lifestyle changes
Lifestyle changes are an important part of managing PCOS and improving your chances of getting pregnant. By making healthy lifestyle changes, you can improve your overall health and well-being, and you can also help to regulate your hormones and improve your fertility.
- Diet
Eating a healthy diet is essential for managing PCOS and improving your fertility. A healthy diet for PCOS includes plenty of fruits, vegetables, and whole grains. It should also be low in saturated fat, cholesterol, and sodium.
- Exercise
Exercise is another important part of a healthy lifestyle for women with PCOS. Exercise can help to improve insulin sensitivity, reduce stress, and promote weight loss. All of these factors can help to improve your fertility.
- Weight loss
If you are overweight or obese, losing weight can help to improve your fertility. Weight loss can help to improve insulin sensitivity, regulate your hormones, and reduce inflammation. All of these factors can help to improve your chances of getting pregnant.
- Stress management
Stress can worsen PCOS symptoms and make it more difficult to get pregnant. Learning how to manage stress can help to improve your overall health and well-being, and it can also help to improve your fertility.
Making lifestyle changes can be challenging, but it is important to remember that these changes can have a significant impact on your health and fertility. By making healthy lifestyle changes, you can improve your chances of getting pregnant and having a healthy baby.
Medications
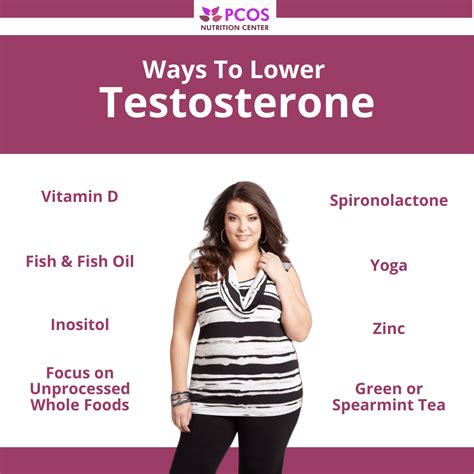
Medications play a crucial role in managing PCOS and improving fertility in women with high testosterone levels. Various medications target different aspects of PCOS, from hormonal imbalances to insulin resistance and ovulation induction.
- Ovulation induction medications
These medications, such as clomid and letrozole, stimulate the ovaries to produce and release eggs, addressing the common issue of ovulation irregularity in PCOS.
- Hormonal birth control
Birth control pills containing estrogen and progestin can regulate menstrual cycles, reduce testosterone levels, and improve insulin sensitivity, creating a more favorable environment for conception.
- Insulin-sensitizing medications
Metformin, a common medication for type 2 diabetes, can improve insulin sensitivity in women with PCOS, reducing the negative effects of insulin resistance on fertility.
- Anti-androgen medications
Spironolactone and flutamide are anti-androgen medications that can lower testosterone levels, potentially improving ovulation and fertility outcomes.
Medications provide effective means to manage PCOS and enhance fertility in women with high testosterone. By addressing hormonal imbalances, regulating menstrual cycles, and improving insulin sensitivity, these medications increase the chances of successful pregnancy.
Surgery
Surgery may be considered for women with PCOS and high testosterone who have not responded to other treatments. Surgical procedures aim to improve ovulation and fertility by addressing underlying factors contributing to PCOS.
- Ovarian drilling
This laparoscopic procedure involves making small incisions in the ovaries to reduce the number of follicles and restore ovulation.
- Wedge resection
A portion of the ovary is removed to decrease the production of testosterone and promote ovulation.
- Laser ovarian drilling
A laser is used to create small burns on the ovaries, stimulating ovulation without the need for incisions.
- Hysteroscopic metroplasty
This procedure aims to correct uterine abnormalities, such as a septum or polyps, that may interfere with implantation and pregnancy.
Surgery can be a successful option for women with PCOS and high testosterone who have not achieved pregnancy with other treatments. However, it is important to weigh the potential risks and benefits before considering surgery.
Assisted reproductive technologies
For women with PCOS and high testosterone who have not been successful with other treatments, assisted reproductive technologies (ART) may be an option. ART procedures involve manipulating eggs, sperm, or embryos to achieve pregnancy.
- Intrauterine insemination (IUI)
IUI involves placing sperm directly into the uterus around the time of ovulation, increasing the chances of fertilization.
- In vitro fertilization (IVF)
IVF involves retrieving eggs from the ovaries, fertilizing them with sperm in the laboratory, and then transferring the resulting embryos back into the uterus.
- Intracytoplasmic sperm injection (ICSI)
ICSI is a specialized IVF technique where a single sperm is injected directly into an egg, increasing the chances of fertilization in cases of severe male factor infertility.
- Gestational surrogacy
Gestational surrogacy involves using a surrogate mother to carry and deliver a pregnancy using the intended parents’ eggs and sperm or donor eggs and sperm.
ART procedures can be complex and expensive, and they do not always guarantee success. However, they can offer hope to women with PCOS and high testosterone who have been unable to conceive on their own.
Emotional support
Emotional support is crucial for women with PCOS and high testosterone who are trying to get pregnant. Dealing with the challenges of PCOS, including hormonal imbalances, weight issues, and fertility struggles, can be emotionally taxing. Emotional support can provide a sense of comfort, validation, and encouragement, which can positively impact their overall well-being and ability to cope with the challenges of their condition.
Support groups, online communities, and therapy can offer women with PCOS a safe and supportive environment to share their experiences, learn from others, and connect with individuals who understand their struggles. This can help reduce feelings of isolation and stigma, improve self-esteem, and provide practical advice and coping mechanisms.
Emotional support can also play a role in improving fertility outcomes. Stress can negatively affect hormone levels and ovulation, while emotional well-being and relaxation can contribute to hormonal balance and improve the chances of conception. Therefore, ensuring that women with PCOS have access to emotional support can be an important part of their fertility treatment plan.
FAQs on Getting Pregnant with PCOS and High Testosterone
This section addresses frequently asked questions to clarify aspects and provide insights on getting pregnant with PCOS and high testosterone.
Question 1: What are the main challenges of getting pregnant with PCOS and high testosterone?
Answer: PCOS and high testosterone can disrupt ovulation, making it difficult to conceive naturally. Hormonal imbalances, insulin resistance, and weight management can also pose challenges.
Question 2: What lifestyle changes can improve fertility for women with PCOS and high testosterone?
Answer: Maintaining a healthy weight, eating a balanced diet, exercising regularly, and managing stress can positively impact hormone levels, insulin sensitivity, and overall well-being.
Question 3: What medications are commonly used to treat PCOS and high testosterone?
Answer: Medications like clomid, letrozole, metformin, and anti-androgens may be prescribed to regulate menstrual cycles, stimulate ovulation, improve insulin sensitivity, and reduce testosterone levels.
Question 4: When is surgery considered for women with PCOS and high testosterone?
Answer: Surgery may be an option for those who have not responded to other treatments. Procedures like ovarian drilling or wedge resection aim to restore ovulation by reducing the number of follicles or excess ovarian tissue.
Question 5: What assisted reproductive technologies (ART) are available for women with PCOS and high testosterone?
Answer: ART procedures like IUI, IVF, and ICSI can assist with conception by directly placing sperm into the uterus or fertilizing eggs in the laboratory.
Question 6: Why is emotional support important for women with PCOS and high testosterone who are trying to get pregnant?
Answer: Emotional support provides validation, reduces isolation, and offers coping mechanisms. It can positively impact well-being and potentially improve fertility outcomes by reducing stress and promoting hormonal balance.
These FAQs provide essential information and guidance on various aspects of getting pregnant with PCOS and high testosterone. Understanding these aspects can empower individuals to make informed decisions and navigate their fertility journey.
In the next section, we will delve into managing PCOS and high testosterone during pregnancy, exploring potential risks, adjustments, and necessary care.
Tips for Getting Pregnant with PCOS and High Testosterone
Managing PCOS and high testosterone during pregnancy requires proactive measures to ensure a healthy and successful journey. Here are some practical tips to help you navigate this:
Tip 1: Regular Prenatal Care: Establish regular prenatal appointments with your healthcare provider to monitor your health, adjust medications, and address any concerns promptly.
Tip 2: Glucose Management: Monitor your blood sugar levels closely, as PCOS increases the risk of gestational diabetes. Follow a balanced diet and consult with your doctor about insulin or medication if needed.
Tip 3: Weight Management: Maintain a healthy weight throughout pregnancy to reduce risks associated with PCOS, such as preeclampsia and gestational hypertension.
Tip 4: Exercise and Activity: Engage in regular physical activity as recommended by your doctor. Exercise helps regulate hormones, improves insulin sensitivity, and reduces stress.
Tip 5: Stress Management: Prioritize stress-reducing activities such as yoga, meditation, or spending time in nature. Stress can worsen PCOS symptoms and affect pregnancy.
Tip 6: Medication Adjustments: Your doctor may adjust your PCOS medications during pregnancy to ensure optimal hormone levels and support a healthy pregnancy.
Tip 7: Monitoring Fetal Growth: Undergo regular ultrasounds to monitor fetal growth and development. PCOS may increase the risk of intrauterine growth restriction.
Tip 8: Postpartum Care: After delivery, continue follow-up care to manage PCOS and address any long-term effects it may have on your health.
Following these tips can help you manage PCOS and high testosterone during pregnancy, increasing your chances of a healthy pregnancy and delivery. These proactive measures contribute to a positive pregnancy experience and the well-being of both mother and baby.
In the final section, we will discuss the importance of self-care and support for women with PCOS and high testosterone throughout their pregnancy journey.
Conclusion
Navigating pregnancy with PCOS and high testosterone requires proactive management and tailored care. This article has explored the challenges, treatment options, and self-care strategies to empower individuals on this journey. Key points emphasized include:
- Understanding the hormonal and metabolic complexities of PCOS during pregnancy is crucial for effective management.
- Regular prenatal care, medication adjustments, and lifestyle modifications are essential to mitigate risks and promote a healthy pregnancy.
- Emotional support, stress management, and patient advocacy are integral to the well-being of women with PCOS throughout their pregnancy.
Remember, managing PCOS and high testosterone during pregnancy is a collaborative effort between individuals and their healthcare providers. By embracing a proactive and informed approach, women with PCOS can increase their chances of a healthy pregnancy and the well-being of their child. This journey requires resilience, self-care, and access to comprehensive support systems.